Now Accepting New Patients!
Welcome to Health Connections DPC
We believe better health starts with better connections—
to your doctor,
your body,
and your goals.

Personalized

Same / Next Day Care

Compassionate

Affordable
🤝 PERSONALIZED PRIMARY CARE AND IMMIGRATION EXAMS — without the rush or red tape.
Direct Primary Care
🕐 Longer Visits - We take the time to talk about what matters—without the rush or 15-minute time limits.
📞 Direct Access to Your Doctor - No call centers. Call or send me a message directly.
📅 No-Rush Appointments - Same or next-day visits when you’re sick or need help - without waiting weeks - in-person or from home.
🍎 Weight and Lifestyle Support - Real help with nutrition, movement, sleep, and stress—no crash diets or one-size-fits-all advice.
❤️ Chronic Disease Management - Personalized support for blood pressure, diabetes, menopause, anxiety, and more.
💉 No Insurance Hassles - No copays, no deductibles, no surprise bills. Simple, transparent pricing every month.
🩺 A Doctor Who Knows You - Build a lasting relationship with a physician who listens, cares, and walks with you on your health journey.
Immigration Medical Exams (I-693)
💬 USCIS Designated Civil Surgeon On-Site-
Your exam is done by Dr. Cynthia Villacis—no outsourcing, no guesswork.
🌎 We speak Spanish and English fluently - and provide phone interpreter for other languages.
You’ll feel heard, respected, and understood.
⏱ Fast Appointments — usually within 1 week -We know your time and deadlines matter.
💰 Affordable Pricing for Uninsured Patients - Transparent fees, no surprise charges.
📆 Saturday appointments - Designed to fit your family’s schedule - only for our immigration patients.
🩻 One-Stop Service: Labs + Vaccines in Office - at reduced prices for uninsured, billed to insurance if insured.
📝Complete and Accurate Paperwork - Your Form I-693 is carefully completed, signed, and sealed to meet all USCIS requirements the first time.
🫶 Over 1,000 individuals and families helped - with calm, friendly, professional care every step of the way.
Whole-Person Primary Care for Adults in Their 30s, 40s, and Beyond
Personalized care for women and men navigating life's transitions—be it managing blood pressure, addressing weight concerns, coping with stress, adjusting to hormone therapy, navigating menopause or andropause, planning for the future, or just want a doctor who listens - we're here.
We proudly care for adults of all backgrounds, bodies, identities, and immigration statuses.
Book a Meet-and-Greet or Get Started with DPC
Schedule a free consultation to meet your potential doctor and learn if we're the right fit for your health journey. - or if you're ready to join schedule your 1st appointment!
Download our e-book on "How to get the most out of your primary care visit"
How is Health Connections DPC different?
Areas of Care
WELLNESS VISITS
IMMIGRATION MEDICAL EXAMS
METABOLIC HEALTH and OBESITY MEDICINE
LIFESTYLE MEDICINE
MENTAL HEALTH
WOMEN'S / SEXUAL HEALTH
SICK CARE
FAMILY CARE
I have been under Dr. Villacis’ care for almost 2 years. Her level of care, her compassion, and her medical knowledge is unsurpassed. She is easy to talk to, and she spends the time necessary to help me with whatever medical issues I may have. I’m 54 years old, and can guarantee that I spoken to her more in the short time I’ve been under her care than all of the other doctors I’ve seen in my life...combined! She never rushes me and I don’t feel like I’m on an assembly line when I’m in her office. I know that I am not an “easy” patient, but Doc works with my sometimes bad attitude and explains things to me in terms I can understand. Signing up to be a patient in her practice was by far the best decision I’ve ever made for my health and well-being.
-Jon, Google Review
I would highly recommend Dr. Villacis and her team. The doctor and her staff take their time with the care of their patients and leave you feeling satisfied with their treatment. Dr. Villacis has a great bedside manner and I would highly recommend this doctor and her staff. Everyone is professional, attentive and patient.
-Michelle, Google Review
I can't recommend Health Connections Direct Primary Care enough! Dr. Cynthia and her team are fantastic. They provide personalized, attentive care that goes above and beyond.
Scheduling appointments is a breeze, with convenient in-person and video options. Once there, wait times are minimal, and Dr. Cynthia takes all the time needed to listen to concerns and develop a plan.
The best part? Their direct primary care model means affordable monthly membership with no hidden co-pays or surprise charges. It's refreshing to have a doctor's office that truly prioritizes my health, not insurance hassles.
If you're looking for a top-notch primary care experience, look no further than Health Connections DPC!
- Moe, Google Review

Pricing
PRIMARY CARE
Monthly Payments
$95/mo
per single adult or child
$30/mo
per child with enrolled adult
$210/mo
for a family of four
$180/mo
for two adults
PLUS
$200
First Visit Fee per person
Includes:
-All in-office visits and testing
-Same/next day office visits
-Direct messaging with your doctor
-Video visits
-Discounted prices on labs and vaccines
Please note - we do NOT bill insurance and CAN NOT see patients with KY Medicaid or Medicare
Yearly Payment
$1045
for 1 year per single adult or child
$330
for 1 year per child with adult
$2310
for 1 year per family of 4
$1980
for 1 year for 2 adults
Pay upfront and get 12th month free AND no first visit fee!
Includes:
-All in-office visits and testing
-Same/next day office visits
-Direct messaging with your doctor
-Video visits
-Discounted prices on labs and vaccines
Please note - we do NOT bill insurance and CAN NOT see patients with KY Medicaid or Medicare
Designed for people who do not want to have an on-going doctor/patient relationship.
One-Time Visit
$300
for 1 visit
Please note - we do NOT bill insurance and CAN NOT see patients with KY Medicaid or Medicare
EXCLUDES:
-follow-up care, messaging, or prescriptions for more than 1 month of medicines.
-Does not include in-office testing
-Same/next day office visits not guaranteed
💬 Wondering if it’s really the right fit for you? We get that. Here are some of the most common questions people ask before they join.
What is Direct Primary Care (DPC)?
DPC is a membership-based model where you pay a monthly fee for unlimited access to your doctor—without dealing with insurance, copays, or rushed visits.
Do you take insurance?
We don’t bill insurance. Instead, your membership covers your care directly. Many of our patients keep a basic plan or healthshare for emergencies and use DPC for everything else.

What if I just need an immigration medical exam?
We offer complete I-693 immigration exams, including labs and paperwork. You don’t need to be a regular patient to schedule one. Learn more →

Do you see kids?
We primarily focus on adult care, but we do provide basic care for children of our members—like sick visits and physicals.

What’s the best way to get started?
The easiest way is to schedule a free 15-minute call to see if we’re a good fit. We’d love to meet you and answer your questions.


Our Physician and Team
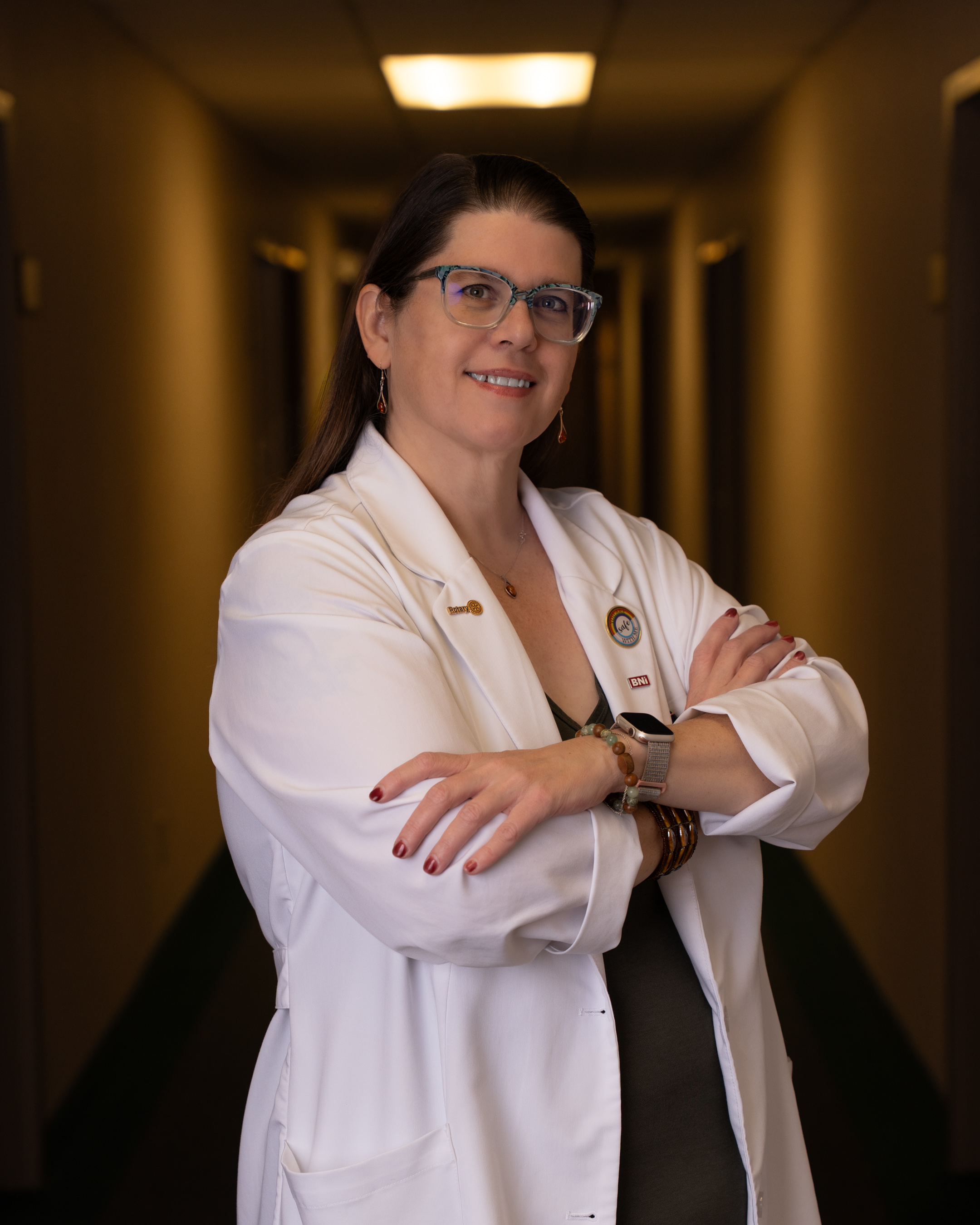
Dr. Cynthia Villacis, MD
Bilingual Family Physician, Civil Surgeon and Life Coach
I’m Dr. Cynthia Villacis, a family doctor with over 20 years of experience — and someone who’s walked many of the same health journeys as my patients. I’ve faced struggles with weight, blood sugar, stress, and sleep, and I know how frustrating it is to feel like you’re doing everything right and still not getting answers.
That’s why I created Health Connections DPC — to offer care that’s personal, judgment-free, and focused on the whole you. I take time to listen, look at root causes, and help you build a plan that fits your life. I also proudly serve a diverse, inclusive community — including immigrants, LGBTQ+ individuals, and Spanish-speaking families — with compassion and respect.
I completed my residency in Family Medicine in 2002 — the same year my second child was born — and I’ve spent over two decades helping people manage chronic conditions like diabetes, hypertension, and obesity through a root-cause approach grounded in lifestyle medicine. I’m also board certified in addiction medicine and have a special interest in mental health, women’s health, and immigrant health.
For many years, I worked in a busy community health center. But I found that 10-15 minute visits weren’t enough to make the kind of meaningful impact I wanted — especially for patients dealing with stress, mood struggles, weight gain, or hormonal changes. That’s why I opened my own practice in 2017, offering longer visits, easier access, and more time to actually connect and care.
My practice is fully bilingual in English and Spanish. I learned Spanish while living in Ecuador as an exchange student in 1988 — where I also met my future husband. I’ve had a passion for working with immigrant families ever since, and I’m also a designated civil surgeon, providing USCIS I-693 immigration medical exams in a compassionate, low-stress environment.
Outside the office, I’m a proud mom of two grown kids, wife of 30+ years, and outdoor enthusiast. I enjoy kayaking, yoga, hiking, scuba diving, and exploring new places — and I strongly believe that joyful movement and adventure are possible at any size. I’ve been on my own journey with weight, metabolic health, and self-compassion, which fuels the care I offer my patients.
If you’re looking for a doctor who sees the full picture — body, mind, and lifestyle — and who truly takes the time to listen, I’d love to welcome you to Health Connections DPC.
🎓 Education & Training
Medical School: Wright State University School of Medicine (1999)
Residency: St. Elizabeth Family Medicine, Edgewood, KY (2002)
Undergraduate: Oberlin College, BA in Biology
High School: Sycamore High School, Montgomery, OH + Colegio Ambato, Ecuador (exchange year)
📜 Certifications
-Board Certified in Family Medicine
-Board Certified in Lifestyle Medicine
-Board Certified in Addiction Medicine
-Certified Life Coach (The Life Coach School) and additional training through WellCoaches
👥 Memberships
American Academy of Family Physicians
American College of Lifestyle Medicine
American Society of Addiction Medicine
Northern Kentucky Medical Society

👩💼 Meet Gisselle
Bilingual Medical Assistant & Office Manager
I first joined Health Connections DPC in 2023 and returned in the fall of 2024 after completing my Associate’s Degree in Business. It’s an honor to now serve as both a medical assistant and the office manager, supporting our patients and keeping things running smoothly behind the scenes.
Originally from Puerto Rico, I moved to Kentucky in 2017 and have been dedicated ever since to helping people from all backgrounds feel cared for and understood. As a bilingual team member, I take pride in bridging language and cultural gaps — ensuring that both English and Spanish-speaking patients receive the clear, compassionate care they deserve.
I love learning and am always looking for ways to grow in my role and serve our community even better. Outside of work, I enjoy reading, knitting, and spending quality time with my family — the people who keep me grounded and inspired.

We Celebrate ALL Backgrounds













Facebook
Instagram
LinkedIn
Youtube